(Picture Source: Wikipedia, 2020)
A global health problem needs a global perspective. I am a believer in looking outside of ourselves to connect the dots and to find solutions to big problems. The Opioid Crisis is a big problem. The U.S. has traditionally approached it either as a weakness of character and more recently as a medical condition. Some programs, based on Alcoholics Anonymous, preach abstinence and will therefore judge and exclude people participating in Medication-Assisted Treatment programs. Court systems will often impose a particular treatment program on individuals they process for opioid-related offences. Patients are not treated as individuals and instead are pushed through a one-size-fits-all solution.
There is a push in the U.S. to have primary care clinicians compensate for our current disjointed substance use disorder management system. Many in the medical field want primary care doctors to address patients’ substance use and mental health disorders. Primary care doctors, however, have to go through an eight-hour training in order to be able to prescribe Buprenorphine, a drug used with success to manage withdrawal symptoms. This constitutes a barrier to provide much needed treatment in more rural areas. There is a current movement to remove this regulation (Waters, 2019). In order to understand how this would help, let’s take a look at the French approach to treating Opioid dependence.
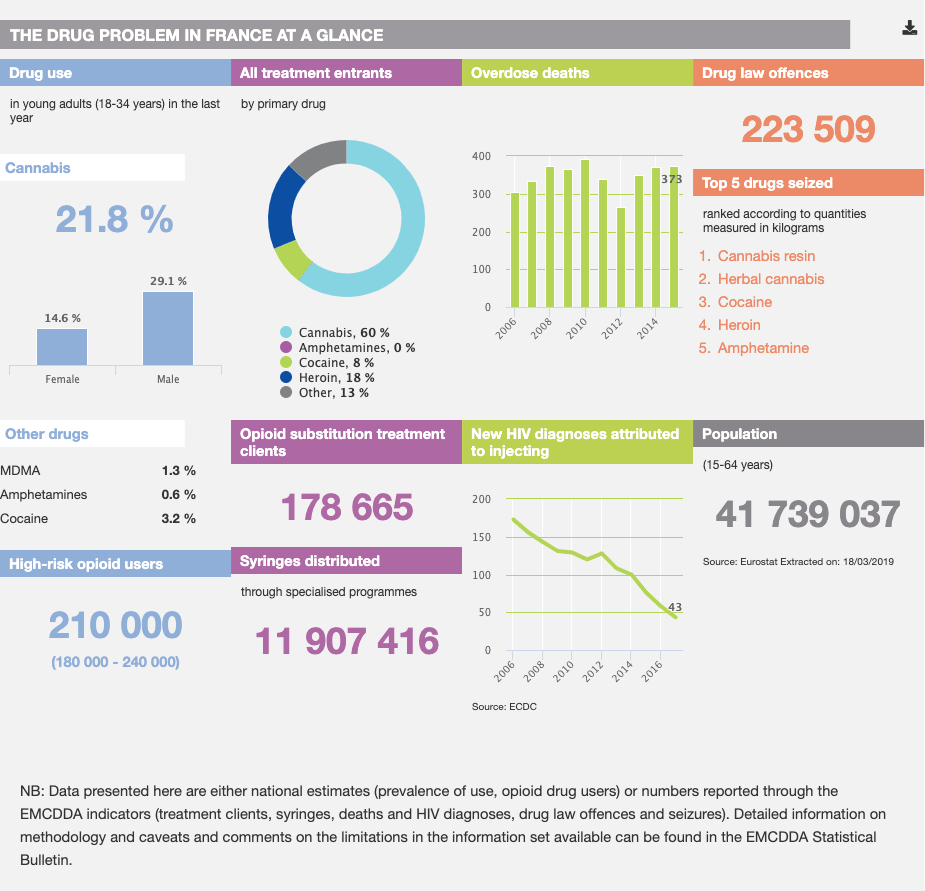
In contrast to the U.S., France places no restrictions on medical doctors prescribing Buprenorphine, no matter their specialty. No additional education is required because it is treated just like any other medicine. This means that primary care doctors can be a resource for patients with substance use disorders, even those in remote locations. Dispensing can be daily, weekly, or every 28 days. French doctors partner with pharmacists for the monitoring of dosage and medicine distribution. France has had a drastic decrease in Opioid related deaths as a result of this access-based approach. Authors Dupouy, Palmaro, Fatséas, Auriacombe, Micallef, Oustric, and Lapeyre-Mestre, state in their 2017 study that, “We found that compared with the French general population, the mortality rate for patients initiating buprenorphine treatment was 3 times higher; at the same time, it was lower than that observed in previous studies among dependent or regular users of opioids.” They compare their results with another study out of Australia that showed similar positive results in the Buprenorphine patient population.
This information from France would suggest that access and removing regulatory barriers for primary care management of SUD patients and the prescription of Buprenorphine should be a priority policymakers in U.S. as well–eliminating the Buprenorphine 8-hour education requirement would be a great start.
Sources
Dupouy, J., Palmaro, A., Fatséas, M., Auriacombe, M., Micallef, J., Oustric, S., & Lapeyre-Mestre, M. (2017, July). Mortality Associated With Time in and Out of Buprenorphine Treatment in French Office-Based General Practice: A 7-Year Cohort Study. Retrieved January 31, 2020, from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5505455/
Waters, R. C. (2019, August 1). In Support of Buprenorphine Deregulation. Retrieved February 8, 2020, from https://www.aafp.org/fpm/2019/0700/p6.html

1 Comment